Epithelial basement membrane dystrophy (EBMD) is a disease where the tissues in the anterior cornea degenerate due to genetic factors. It is also known as map-dop-fingerprint dystrophy, Cogan’s microcystic dystrophy or anterior basement membrane dystrophy. EBMD can cause decreased vision and pain due to recurrent corneal erosions.
Risk factors
The family history of EBMD and age are the important risk factors for the development of the disease. EBMD can be worsened by the following factors: corneal abrasion, contact lens wear, LASIK, implantable contact lens and other intraocular surgery. If you have a known personal or family history of EBMD, you should avoid those factors to prevent the symptoms.
Mechanism
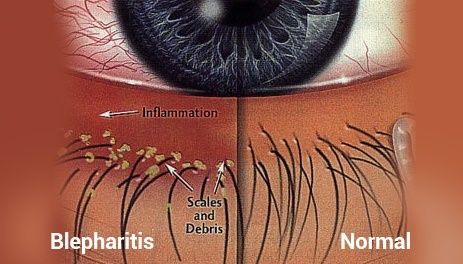
The front outer layer of our eyes is called the cornea while the outer layer of the cornea is called the corneal epithelium. The basement membrane is the innermost layer of the corneal epithelium. In EBMD, abnormal sheets of basement membrane extend into the corneal epithelium, preventing the maturing corneal epithelial cells below to migrate to the anterior surface of the cornea to replace the old cells. The basement membrane becomes thicker. The layers of epithelial cells peel off the basement membrane. It leads to painful recurrent corneal erosions. The thickened basement membrane will form a map or dot or fingerprint pattern that can be observed with a slit lamp. The vision may be blurred if the corneal erosion is located over the pupil.
Diagnosis
Most people with EBMD are asymptomatic until painful recurrent corneal erosion occurs. You will be asked about the blurred vision that comes on and off, foreign body sensation in eyes, recurrent pain in one eye in the middle of the night or upon awakening in the morning. A magnifying device called a slit lamp is then used to examine your cornea (the outer layer of the eye) for the pattern of maps (geographic, sharply demarcated clear zones within light greyish-white areas), dots (irregular patches of greyish white opacities), fingerprints (small clusters of parallel or curved lines) and irregular circles of negative fluorescein staining on cornea under blue light. If the history and slit-lamp examination are positive, then a clinical diagnosis of EBMD can be formed.
Complication
Recurrent corneal erosion and scarring can cause loss of best-corrected visual acuity.
Differential diagnosis
EBMD associated recurrent corneal erosions and scarring are often mistaken as Herpes Simplex or Herpes Zoster keratitis. HSV and HSZ keratitis often cause subepithelial scarring or recurrent corneal erosions. Corneal abrasion and other anterior corneal dystrophies like Reis-Bucklers’ Dystrophy are also differential diagnoses of EBMD
Management
The main concern is to improve the vision and to reduce the recurrence of painful recurrent corneal erosions. Use of lubricating eye ointment or hypertonic saline ointments during the night can prevent corneal erosion. If you are having corneal erosions, the application of antibiotics ointments and bandage contact lenses or patching can promote healing and prevent secondary infection. Topical steroids or oral doxycycline prevents inflammation and infections in people with frequently recurring corneal erosions. To reduce the recurrence of corneal erosions, extended wear of bandage contact lenses, corneal epithelial debridement and surgery can be done. The most recent treatments for recurrent corneal erosions are autologous serum tears or amniotic membranes.
Prognosis
The prognosis is variable but usually poor. Corneal erosions are recurrent and painful. The disease progresses with age. Most people with EBMD experience the symptoms on and off throughout their life.
Book your appointment today at www.mataclinic.com