This article is contributed by Kathie, Optometrist.

Dry eye is not merely dryness in the eyes, it is a complex multifactorial disease. In fact, most patients do not realize its severity until they experience it. People with dry eyes may face difficulty in reading and Visual Display Unit (VDU) eg. computers usage. If you notice your child having frequent eye rubbing, eye irritation and increased blinking rate, dry eye may be suspected. Tears act as a first-line barrier against infection so dry eye that disrupt the tear layers increases the risk of infection in the eyes. Without proper management, severe dry eye leads to inflammation, corneal abrasion, corneal ulcer, corneal scarring and vision loss. There is currently no permanent cure for dry eye but there are several options available for reducing symptoms and preserving vision.
Key pathogenic factors contributing to the vicious circle of dry eye disease. How complex it can be.

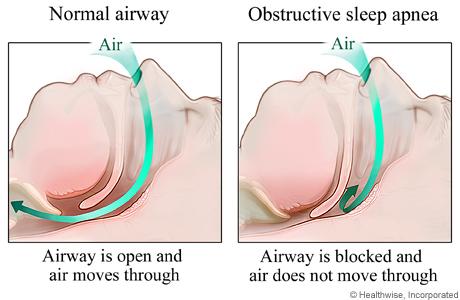
Tear film instability is a hallmark of dry eye and is caused by changes in lipid layer function and in quantity, quality, and availability of tear fluid. Another important factor is the function of transmembrane and secretory mucins, which facilitate the contact between tear fluid and epithelial cells, adversely affected by tear film instability.
The common symptoms reported range from redness in eyes, eye irritation, dryness in eyes, burning sensation, sensitivity to light, foreign body sensation, watery eyes and stringy mucus discharge, to eye fatigue at the end of the day or after long hours of near tasks. Eye pain and temporary blurred vision are also reported. Soft contact lens wearer with severe dry eye may face difficulty and torn lens upon removal of the lenses which may cause eye pain. Therefore, artificial tears are instilled before the removal of the lens in severe dry eye cases. Some patients reported on the usage of artificial tears when symptomatic but the symptoms were temporarily resolved and recurrent. If the topical eye drops used are reported containing preservatives, it may cause increased tear evaporation, leading to dry eye. The causes of the dry eye symptoms are investigated for proper management.
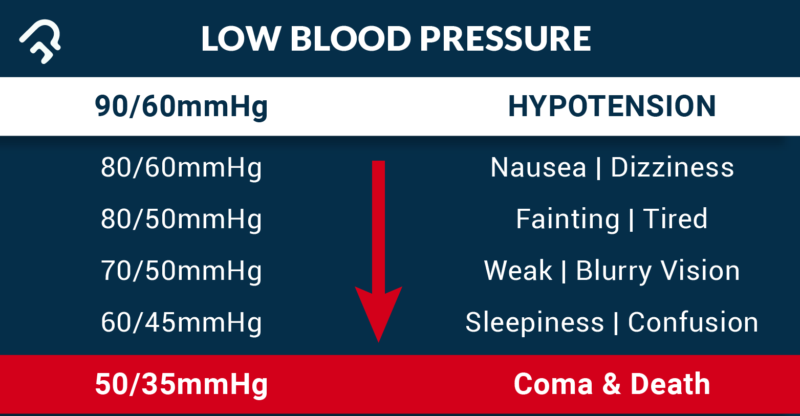
In short, dry eye is a condition marked by inadequate lubrication in the eyes due to insufficient tear production or abnormally increased tear evaporation rate. The patient’s usual working environment should be investigated because long-duration exposure to wind, low humidity, smoke, heat, sunlight, chemical fumes and air-conditioning will increase the tear evaporation rate. For women, hormonal changes due to pregnancy, menopause and intake of birth control pills will cause dry eye as side effect. Allergies, chronic ocular inflammation, skin disease involving eyes and eye glands, refractive surgeries like LASIK and autoimmune disorders like rheumatoid arthritis may be associated with dry eye range from mild to severe stage. Besides, reduced blinking rate and incomplete eye closure (lagophthalmos) increase tear evaporation, leading to dry eye. In addition, medications like antihistamines, nasal decongestants, blood pressure control medication, medication for Parkinson’s disease and antidepressants will cause dry eyes. Long term contact lens wear is often associated with mild to severe dry eye. A diet that is low in Vitamin A or omega-3 fatty acid also decrease tear production and increase tear evaporation, leading to dry eye.

The management of dry eye is mainly aiming to reduce symptoms, to prevent further damage to ocular tissues and to conserve the vision. First, the causative factor and type of dry eye is identified based on a series of procedures. Elimination of causative factors is the first approach. Patient education on the cause and severity of dry eye is important to advise on environmental modification at home and work. Modification of systemic medication is subjected to the physician’s advice. In some cases, the modification on the type and dosage of medications reduces the dry eye symptoms without causing adverse health effects. Discontinuation of contact lens wear is essential while the dry eye treatment is in progress. The treatment requires consistent compliance for a long period. The remaining eyeliner and other eye makeup may clog up the orifices of the meibomian gland, leading to meibomian gland dysfunction and evaporative dry eye. Therefore, make sure all traces of makeup are removed thoroughly from the lid and lashes at the end of the day. Simply drinking more water and taking supplements containing omega-3 fatty acids may help reducing symptoms.
Patients are advised for proper visual hygiene like taking periodic eye breaks during the long task that require visual concentration to reduce eye fatigue and improve the blinking rate. Based on the 20-20-20 rule, looking away from the screen every 20 minutes to look at any object at about 20 feet (6 metres) away for at least 20 seconds relieve dry eye and eye strain. Eye breaks can also be simple closing eyes for 1 to 2 minutes and repeated blinking to help evenly spreading tears over the eyes. The VDU screen should be positioned below user’s eye level to so the user does not require widely opening eyes for viewing. Prevention of exposure of the eyes to the environmental irritants can be done by wearing sunglasses with 100% UV protection and a wrap-style frame or safety glasses at work to protects the eyes against dust, smoke and wind.
The following management is based on type and severity of dry eye cases. For your information, our tears are consisting of three layers; which are the superficial lipid layer to reduce the tear evaporation rate, the middle aqueous layer and the inner mucous layer produced by goblet cells to spread the aqueous layer evenly over the ocular surface. Aqueous tear-deficient dry eye is due to low tear production resulting from the failure of lacrimal glands to produce a sufficient aqueous layer of tears. Evaporative dry eye has a strong association with meibomian gland dysfunction which results in reduced production of the lipid layer of tears and increased evaporation of tears.
For aqueous tear-deficient dry eye, artificial tears or over-the-counter lubricating eye drops can be used for controlling mild symptoms. Non-preservative eye drops are more recommended and safer in avoiding eye irritation. It comes in multiple single-use vials. Eye drops can be used at any time and will not interfere with vision but thicker eye ointment can cloud vision and is better used before bedtime.
Evaporative dry eye is associated with meibomian gland dysfunction that is marked by notching of the lid margin, telangiectasia, capping of meibomian gland orifices, reduction of orifices and foamy secretion upon pressure. Blepharitis and other associated inflammation may be present. The main goal should be to reduce lid margin inflammation. This will include lid margin hygiene, corticosteroids/antibiotic ointment and eye drops, together with the use of tear substitutes in order to allow a more efficient control of the tear film stability. Warm compress and lid hygiene can be performed. A clean cloth wetted with warm water is applied over the affected eye for 5 minutes. The cloth is then rewetted with warm water and is used to rub over the eyelid and base of the eyelash to soften and remove any debris and clogs present. Baby shampoo or any mild soap can be used as a cleanser and is gently massaged over the closed lid and the base of eyelashes with clean fingertips, followed by thorough rinsing. Meibomian gland expression can be performed as an in-office procedure to squeeze the clogged contents from the meibomian glands with a forceps-type of device. The significant pressure applied may cause short term discomfort but the significant effect on resolving dry eye symptoms make it tolerable.
Based on the severity of symptoms, the treatment may be different. The frequency and type of eye drops are depending on the severity of the dry eye symptoms. For asymptomatic dry eye, follow up and monitoring is important. If clinical findings show mild meibomian gland dysfunction, warm compress and lid hygiene can be done. If the symptomatic eyes do not or poorly respond to topical lubrication therapy, tiny silicone punctual plugs can be applied to the lacrimal punctum to prevent tear drainage and conserve the natural tears and artificial tears. Xiidra is the newest medication in a new class of drugs, called lymphocyte function-associated antigen 1 (LFA-1) antagonist, approved by the FDA for dry eye disease. The generic for Xiidra is Lifitegrast. This is the latest since Restasis which was launched in 2003.
In conclusion, this article has demonstrated that dry eye ought to be taken seriously. Be aware of the dry eye symptoms in daily life for early diagnosis and treatment. Patient has to be realistic about the treatment results because it will be a long process. Patient’s compliance and follow-ups are required for better results. Luckily, dry eye rarely causes permanent vision loss.


Recent Comments